Applying Health Equity-informed Planning to Operations in Niagara Region
THE PROJECT
In 2018, Niagara Region Public Health & Emergency Services Department (NRPH&ES) developed a Health Equity Strategic Plan to guide operations and programs run by the health department. However, as health equity is impacted by many aspects of society, part of the Strategic Plan was to engage other departments in the health equity mission as well.
In 2019, an opportunity to influence the broader regional government planning process presented itself. The goal of the Health Equity-informed Planning (HEIP) Project was to ensure that the health implications of non-health-sector projects undertaken by the regional government are fully considered in the assessment and design phases.
BACKGROUND
Located in Southern Ontario between Lake Ontario and Lake Erie, across the Niagara River from New York State, Niagara Region has a population of approximately 485,000. Known for its fruit farms and wineries, Niagara Region also captures several urban centres, including Niagara Falls, St. Catharines, and Welland. The region is governed by two tiers of government – the Regional Municipality of Niagara and 12 local municipalities. Public health is a department of the regional government.
The NRPH&ES has a long history of work on active transportation and environmental health. In 2010, it had an interdisciplinary team that worked collaboratively to influence land use and transportation planning processes in the region with the goal of improving public health.
THE PROCESS
The HEIP project was adopted in November 2020 when the Regional Council amended the Budget Planning By-law to include a health equity clause, namely: “Establish social determinants of health as a consideration in program and budget decisions.”
This clause was added in pursuit of the Regional Council’s priority to become a “Healthy and Vibrant Community”. By including the social determinants of health (SDOH) as an objective in the by-law, the health impact assessments effectively became required considerations in budget decisions.
“The project was supported by Regional Councillors and leadership,” said Kate Harold, Strategic Initiatives Coordinator with NRPH&ES. “There were many contextual factors that helped make this project acceptable. For example, in previous years, there had been a high number of suicides on one of our bridges in Niagara, and a barrier was built to prevent additional deaths. That helped people in the region understand how issues unrelated to the health system – such as transportation infrastructure – can impact public health. Those tragic events helped to make the SDOH real for our councillors and colleagues in other departments.”
The goal of the project is to improve health and reduce health inequities by ensuring that the SDOH are considered when assessing projects and programs proposed by the Regional Municipality.
Under the HEIP Project, all non-health projects undergo a Health Impact Assessment (HIA) that was adapted by NRPH&ES from the World Health Organization’s (WHO) Health Impact Assessment toolkit. The project, which was piloted for the first time in 2021, is currently being coordinated by two NRPH&ES staff – an HIA Coordinator and Kate Harold, the Strategic Initiatives Coordinator.
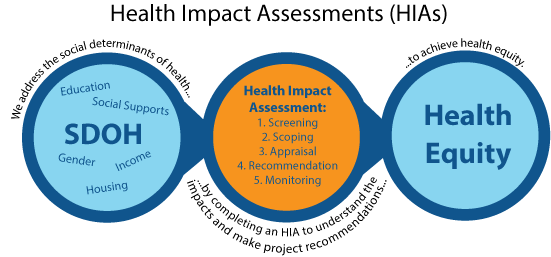
There are five steps to the HIA process: Screening, Scoping, Assessment, Recommendations, and Monitoring.
In the first step, a qualitative scan is conducted by the Project Manager for the project being screened, the two public health staff who coordinate the process, and other public health staff who have expertise relevant to the project. The impact of project actions is rated on a scale of -3 to +3, reflecting its potential to amplify or mitigate negative health impacts on priority populations, for each one of the SDOH.
The SDOH to be considered include: environmental determinants (i.e., air, water, topography and natural heritage), transportation, housing, working conditions, neighbourhood safety, education, access to public services, built environment, social supports, family, food security, and economic development.
The priority populations identified by the Ontario Ministry of Health in its HEIA toolkit are those who can be disproportionately affected. The screening scores are summated to determine whether an HIA is needed, and if so, whether a rapid, intermediate or comprehensive HIA should be conducted.
A rapid HIA is a desktop exercise involving secondary data that already exists. An intermediate HIA is one that involves the collection of primary data and community stakeholder engagement as well as secondary data. A comprehensive HIA involves the extensive collection of both qualitative and quantitative primary data, as well as secondary data, structured community stakeholder engagement, and project-specific funding for a more work-intensive and thorough approach.
OUTCOMES ACHIEVED
In 2021, 11 projects were screened for the 2022 budget. It was decided that an HIA would have low value for four which had few and limited potential health impacts identified. HIAs were recommended for seven projects. Two of the pilot HIAs had been completed as of May 2022. The screened projects were related to transportation systems, waste management, water treatment and affordable housing.
Using a road reconstruction project in St. Catharines as an example, the HIA generated a number of recommendations that complemented the environmental assessment. Driven in part by the presence of three schools and four adult living facilities in the study area, the HIA recommended adjustments to encourage active modes of transportation, improve the safety of pedestrians and cyclists, and increase access to services.
For example, the HIA recommended:
- fully segregated active transportation facilities;
- a continuous sidewalk network throughout the area;
- appropriate signage, lighting and line painting throughout the study area;
- education on the safe use of Two-Way Left Turn lanes and cycling facilities; and
- promoting connections to public transit.
“It is our hope that HEIP and the HIA tool will improve health, reduce health inequities, and as a whole, decrease our negative impact on air quality, water quality, and the climate,” offered Kate. “In fact, we are hoping that it might actually improve our impact on the environment”.
NRPH&ES considers the HEIP a success to date because it has ongoing support within regional government:
- Regional Council has approved funding to make the HIA Coordinator a permanent position in the 2022 budget;
- the regional government’s interdepartmental working group has been extremely supportive; and
- there are discussions about how best to support the 12 local area municipalities with the integration of health equity into their operations.
LESSONS LEARNED
In order for an innovative policy to be adopted at the municipal level, a highly regarded champion is needed to make the case.
“Niagara Region’s Acting Medical Officer of Health, Dr. Mustafa Hirji, is a passionate advocate for health equity and the application of the SDOH to decision-making,” noted Kate. “Over the years, he has worked to educate Regional Councillors and municipal leadership about the SDOH and the need to address health inequities. He led the creation of the Health Equity Strategic Plan within NRPH&ES, and when Regional Council sought a way to build its vision to create a “healthy and vibrant community” at the start of its term, he seized the opportunity to sell them on health impact assessments as a way to achieve their goal.”
It is easier to get an innovative policy adopted when there are other jurisdictions that are doing the same thing. It was helpful for Niagara Region to know that the Province of Quebec and the City of Vancouver are utilizing HIAs for land use and transportation planning processes. With permanent funding and a by-law requiring their use, NRPH&ES has moved the regional government onto a trajectory that improves health for the long term.
Prepared by Kim Perrotta, MHSc, Executive Director, CHASE
Last modified: July 20, 2022

